Ulcerative Colitis
What is Ulcerative Colitis ?
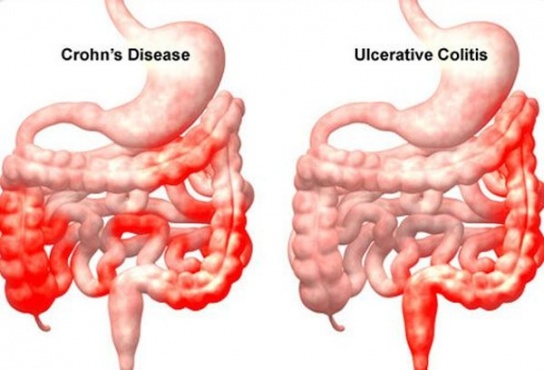
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in your large intestine. Ulcerative colitis affects the innermost lining (mucosal lining) of the large intestine (colon and rectum). Treatment can greatly reduce signs and symptoms of the disease and bring about long term remission. However the patient in remission requires life long treatment and follow up. Ulcerative colitis symptoms can vary, depending on the severity and extent of inflammation. Therefore, doctors often classify ulcerative colitis according to its location/ extent. The patient may have the following signs and symptoms. Diarrhea (often with blood or pus) Rectal bleeding - passing blood with stool Abdominal pain and cramping, Rectal pain with urgency to defecate. Weight loss, fatigue, Fever, Some patients may have symptoms in other parts of the body apart from intestine like joint Pains, backache, inflammation of the eyes, mouth and skin ulcers and liver inflammation. Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission. However, some patients may have very severe course leading to need for surgery. Long-term disease may lead to development of colon cancer in some patients. Therefore, in these patients require periodic check up (surveillance)
Lifestyle Modification
During acute phase of diarrhoea high fiber diet should be avoided. Lactose containing foods (milk and milk products) may also be restricted. when symptoms are well controlled (remission) normal diet is advisable.
- Avoid foods and drinks that trigger symptoms Limit or reduce stress in your life
- Although stress doesn't cause inflammatory bowel disease, it can make your signs and symptoms worse and may trigger flare-ups. Try participating in an exercise, yoga, or meditation program.
- Take your medicines exactly as your doctor prescribes
- Medicines are essential even when the symptoms are well controlled to maintain disease in remission. Regular follow - up and investigation as per your doctor's recommendation is needed.
What type of tests are needed to evaluate Ulcerative Colitis ?
Ulcerative Colitis is diagnosed by examining the mucosal lining of large intestine by colonoscopy. To help confirm a diagnosis of ulcerative colitis, your doctor may advised blood/stool tests in addition to colonoscopy.
- Colonoscopy - This exam allows your doctor to view your entire colon using a thin, flexible, lighted tube with an attached camera. During the procedure, your doctor will take small samples of tissue (biopsy) for laboratory analysis. A tissue sample can help to confirm the diagnosis.
- CT scan - A CT scan of your abdomen or pelvis may be performed if your doctor suspects a complication from ulcerative colitis or inflammation of the small intestine. A CT scan may also reveal extent of the inflamed colon.
- Blood tests - Your doctor may suggest blood tests to check for anaemia/ infection.
These are only a few of the known orthopedic disorders. There are as many treatments for orthopedic disorders as there are problems and injuries in the muscles, ligaments and joints.
- Stool sample - A stool examination can help rule out other disorders, such as infections caused by bacteria, viruses and parasites.
- X-ray - If you have severe symptoms, your doctor may perform an X-ray of abdomen to rule out serious complications, such as a perforated colon.
- Flexible sigmoidoscopy - Your doctor may perform limited examination of colon (sigmoidoscopy) to examine the rectum and sigmoid (the last portion of your colon) if the colon is severely and sigmoid (the last portion of your colon ) if the colon is severely inflamed or during follow up.
